CONDITIONS
Uterine polyps
Uterine polyps
What are polyps?
A polyp is usually when a small part of the inner lining (mostly the mucous membrane) comes out from the surface in the body, formed by growth of tissue there.
A small piece of the inner lining coming out from the body’s surface. That’s a polyp—a growth of abnormal tissue.
What are Uterine Polyps?
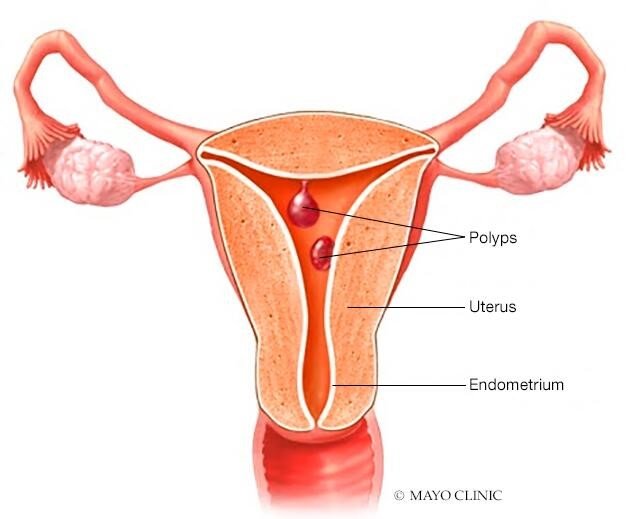
Although uterine polyps may be diagnosed at all ages, most uterine polyp cases are found between the age of 40 to 49 years old. Sometimes, younger people can get them, too. Basically, uterine polyps are most common in people undergoing or undergone menopause.
Uterine polyps can be either one or many and they usually stay within the uterus. It can also happen that they can slip through the opening of the uterus (cervix) into the vagina.
Generally, polyps are noncancerous (benign). However, it’s essential to be cautious, as some can be cancerous or have the potential to turn into cancer (precancerous polyps) Some reasons that may increase the risk of developing cancerous polyps include –
- Age greater than 60,
- Large-sized polyps,
- Menopause status,
- Condition such as
polycystic ovarian syndrome (PCOS) (a condition where multiple cysts develop in a reproductive organ known as ovary)
The exact prevalence of uterine polyps is not known but it is found that half the women who have abnormal bleeding, may have uterine polyps and 35% of infertility cases have uterine polyps.
Symptoms of Uterine Polyps
There are no immediate, noticeable symptoms of polyps, especially if they are small or only one is present. Please discuss the following symptoms with your doctor to check for polyps
- Irregular periods when you can’t predict their timing, length, or heaviness.
- Heavy periods
- Bleeding or spotting between periods
- Vaginal bleeding after menopause
- Trouble conceiving (getting pregnant)
What are the symptoms of menstrual disorders?
Symptoms may vary depending on the type of disorder:
- Pain
- Cramping – sudden pain in lower stomach due to muscles that do not relax after contraction
- Depression
- Headaches
- Emotional distress
- Bloating or fullness in the abdomen
Complications of Uterine Polyps
Most uterine polyps aren’t cancerous, but they can turn into cancer, especially during menopause (when the period stops). Polyps might also affect fertility, leading to miscarriage or difficulty getting pregnant. They interfere with a crucial conception process—the attachment of a fertilized egg to the uterus wall (implantation). They can also block fallopian tubes or the cervix.
While removing polyps is suggested to aid pregnancy, clear proof of its effectiveness is lacking. It’s best to let the doctor decide
What are the causes of Uterine Polyps?
Why women get uterine polyps, is not very well known, but it may be linked to changes in the hormonal level.
During each monthly period, hormone levels fluctuate, thickening the uterus lining, which sheds during menstruation. Polyps form when there’s excessive growth in this lining, often more common during menopause due to estrogen level changes.
A higher risk of developing uterine polyps may be because of:
- Obesity
- High blood pressure
- The breast cancer drug tamoxifen (it is said that around 20% to 35% of females develop polyps due to continuous therapy)
How does the doctor know it is uterine polyps?
Diagnosis
Tests include:
Transvaginal ultrasound: A doctor uses a small device inside the vagina, like a thin wand, to take pictures of the uterus using sound waves. It’s a painless procedure to check for any issues
Hysterosonography or sonohysterography: This is another procedure, often done alongside transvaginal ultrasound. A thin tube called a catheter is placed in the vagina and filled with salt water to expand the uterus, providing a clearer ultrasound picture
Hysteroscopy. A thin, flexible, lighted telescope, called a hysteroscope, is inserted through the vagina and cervix and into the uterus. This allows the doctor to view the tissue lining (endometrium) and, if needed, remove polyps using specialized tools
Endometrial biopsy. A small piece of tissue from the lining of uterus, called the tissue sample, is sent to a lab to test it for cancer cells. This process is called biopsy.
Curettage: In an operating room, a metal instrument called a curette, with a small loop on one end, is used to take a tissue sample or remove polyps from the uterus. Before the exam, some antibiotics, pain relievers, or medicines may be given to dilate the cervix.
Uterine Polyps Treatment
Depending on your case, your doctor might recommend:
Wait and Watch: If there are no symptoms, treatment may not be needed, as the polyp might go away on its own. However, if a woman is past menopause or at higher risk for uterine cancer, removal is often recommended.
Medications: Medications usually are given to control the hormone levels. These may shrink polyps and ease symptoms, like heavy bleeding. The symptoms often return when medicine is stopped but polyps may or may not develop.
Surgery: As mentioned above, doctors can usually remove polyps during the same procedures that are used to diagnose them, such as hysteroscopy or curettage. Instead of making a cut in the stomach, they can insert a curette or other surgical tools through the vagina and cervix to take the polyps out.
Modern-day methods are sophisticated and can be done as outpatient procedures (admission to hospital is not required). However, if the polyps are detected as cancerous, surgery may be required to take out your entire uterus. This procedure is called hysterectomy.
Uterine Polyps Prevention:
References
- Mayo Clinic. (Nov 13, 2023). Uterine polyps. https://www.mayoclinic.org/diseases-conditions/uterine-polyps/symptoms-causes/syc-20378709
- Nijkang NP, Anderson L, Markham R, Manconi F. Endometrial polyps: Pathogenesis, sequelae and treatment. SAGE Open Med. 2019 May 2;7:2050312119848247.
- Diana Reese. (Nov 13, 2023). Uterine Polyps. https://www.webmd.com/cancer/cervical-cancer/uterine-polyps
- Mansour T, Chowdhury YS. Endometrial Polyp. [Updated 2023 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557824/
- Cancer Council (Nov 13, 2023) https://www.cancer.org.au/polyps









